Stem Cell Activation To Regenerate Spinal Discs and Joint Cartilage
It is an exciting time if you suffer from joint or spinal pain. There are options to help avoid cortisone injections or surgery. Regenerative or “stem cell” medicine is a rapidly growing field of medicine that seeks to utilize our body’s own natural ability to heal itself and repair our damaged tissues and organs. We have had the healing power all along, just like Dorothy could have made her way back to Kansas.
How does this work? Stem cells, and also stem cell-based therapies work to reduce accumulated chronic inflammation. This harmful inflammation serves to degenerate our tissues. Alternatively, regenerative medicine approaches work to return our cell’s programming to one that fights against inflammation as a more youthful person would. Although we need to create inflammation as part of our defense mechanism to fight infections and other threats, as we age, our cells, including our stem cells become much less efficient at turning off the anti-inflammatory process, which then leads to chronic inflammation (degenerative) cellular activity. This chronic inflammation causes tissue degeneration. That is the essence of aging.
By awakening our sleepy and aging stem cells, we can achieve our goal of restoring the structural integrity and function of discs in the spine and the cartilage of the joints throughout the body. Degeneration of our cartilage tissues causes reduced moisture and flexibility of discs and joints, loss of volume of the cartilage, and less self-repair (regenerative) activity. This leads to osteoarthritis or “bone on bone” conditions.
Think about it. Our bodies once had the youthful ability to heal themselves rapidly without ongoing chronic inflammation. Regenerative medicine works by tapping back into those cellular activities which had become quiet with age. Keep reading to learn more!
Overview of Disc Regeneration
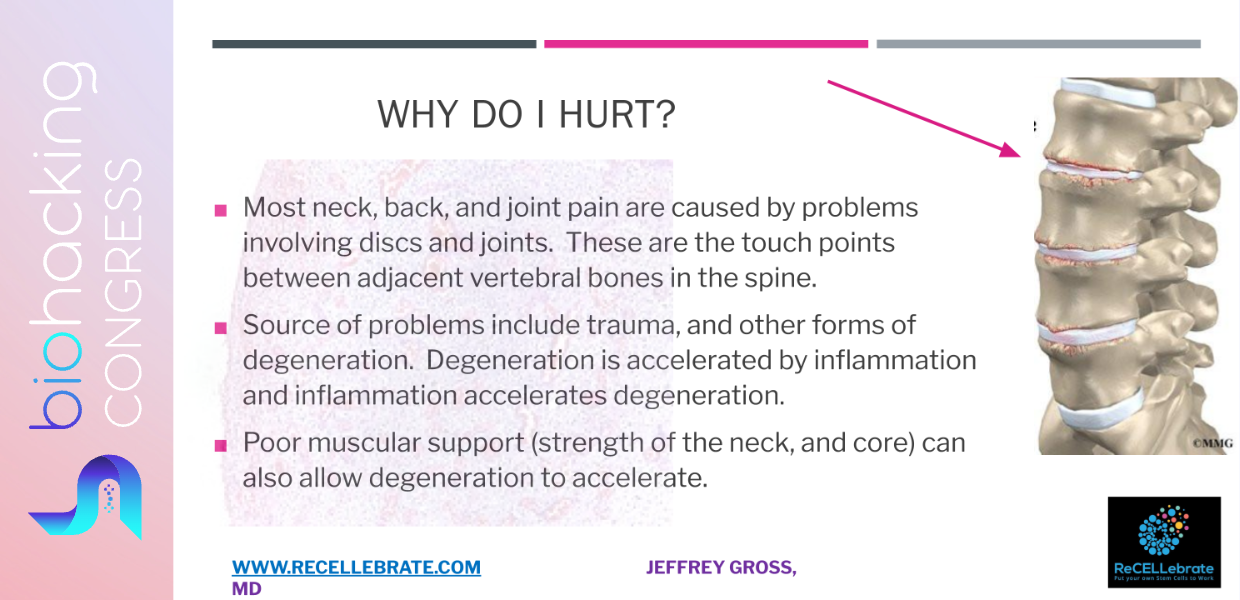
The spine consists of vertebrae (spinal bones) which are connected and supported by intervening discs. These discs act as shock absorbers and help to maintain the spine’s specific flexibility and stability. When the discs become damaged (including inflamed), they become degenerated, which we call “disc degeneration.”This degeneration has the hallmarks of loss of height (they become flatter), loss of water (they become dryer), and loss of cartilage-based proteins (they lose their elastic and cushioning properties).Disc degeneration can cause pain, stiffness, and can limit mobility.We all either have back pain or know someone that suffers from symptoms of spinal degeneration, when it becomes bad enough.
Disc REgeneration (the opposite of DEgeneration) is a restorative process by which degenerated discs are encouraged to repair themselves by producing more of the protein components of cartilage that improve the hydration and cushioning between the spinal vertebral bones. This process is based upon injecting regenerative biologic factors to increase the local stem cell activity. Enhancing the local cellular activity to a more youthful (and anti-inflammatory) state encourages the production of proteins the cartilage needs to function better as well as to reduce pro-inflammatory (degenerative) proteins. This process affects local and neighboring cells. The goal of disc regeneration is to restore the structural integrity of the discs and relieve pain and stiffness.
Other joints, such as the knees, are subject to the same degenerative and inflammatory changes, particularly those that bear weight. Similarly, activating our own stem cells allows for a reversal of inflammatory degeneration on the joint, working to regenerate the cartilage tissues within a joint. The most commonly published examples of joint regeneration with the use of stem cells, is in relation to knee meniscus regeneration. Addressing discs and joints in this way can help reduce the need for spinal and joint surgeries, such as joint replacement.
Current State of Regenerative Medicine for Disc and Joint Regeneration
A variety of techniques are being used to assist with disc and joint regeneration, with the most useful approach being stem cell activation of the nearby bone marrow, where our stem cells are voluminous. The bone on either side of a joint (or spinal disc) is referred to as “subchondral” bone. This is a source of nutrients, blood supply and protein production to the joint or disc. Regenerative biologics to re-awaken our own stem cells are delivered to the subchondral bone. Studies show that these local bone injections, where our most active stem cells exist, are superior to joint injections. There are studies with patients being followed for over 15 years showing the ability to reverse the need for joint replacement with this technique.
Stem cells can be delivered to the subchondral bone to invigorate the cartilage healing process. Stem cells are master cells in our body that can take on the role or characteristics of nearly all other cells in the body through a process of “differentiation.” These cells are the most youthful cells and have a longer cell life, being able to divide more times than our aging differentiated cells. Our stem cells give off both their own growth factors (like those from PRP) and also provide signaling to our other cells and our own sleepy stem cells through small cell-to-cell communication packets called extracellular vesicles (“exosomes”). These growth factors and exosomes rally our own cells into a healing and “anti-inflammatory” mode. This is a youthful and regenerative mode that slows with age. Luckily now, it can be re-ignited.
Stem cells can be harvested from our own body (usually from fat or bone marrow) or can come from someone else. Starting with our own body as the source, stem cells have to be concentrated down to get enough of an effect. Plus, the best stem cells are in our bone marrow, and they are painful to harvest. Fat sources are less painful to harvest, but those cells are affected by undesirable inflammatory cellular pathways and programming. For best results, it makes sense to avoid aged stem cells when trying to obtain a youthful, healing, and regenerative response.
This is where young sources of stem cells come in. The most youthful sources are “perinatal” being obtained from the remnants of a c-section birth. After a baby is delivered by C-section, the elements such as amniotic fluid, placenta, and the umbilical cord can be saved (instead of thrown out). Using these stem cell products has no negative health impact on the mother or child, and there should be no ethical concerns. Expecting mothers are first screened and consented. The collected regenerative products are tested for infectious diseases.
Being the most youthful, these perinatal stem cells and/or exosomes have the most regenerative and anti-inflammatory healing capacity. They are not affected by the accumulation of years of inflammatory, toxic, and oxidant exposure and degradation. Instead, they have the most robust healing activity. Further, stem cell products from another donor person have largely not been known to create an immune reaction in the recipient. This is because stem cells are “immune-privileged” and they modulate the immune system to the advantage of the person receiving them.
When delivered, these stem cells release exosomes also. Their regenerative activity stems from their communication and encouragement of our target cells to reduce inflammatory (aging) pathways, and to improve pathways of repair, healing, and youthful regeneration. These re-invigorated cells then become better at repairing DNA, making proteins (accurately), and improving metabolism within the cell (like a younger cell or younger person does. Through this effect, cellular programming is flipped from that of pro-degeneration, to that of pro-regeneration. This beneficial cellular activity can last for days or weeks, or longer depending on the dose, strength, and nature of the degeneration or inflammation being addressed.
Stem Cell Assistance for Disc and Joint Regeneration
Stem cell therapy is a regenerative medicine technique that involves the use of stem cells and/or exosomes to help one’s local cells behave in a youthful manner to help repair or replace damaged tissues and organs. Stem cells have the ability to differentiate into other cell types, which makes them an ideal tool for regenerative medicine. In the case of disc regeneration, stem cells can be used to help regenerate damaged discs with new, healthy cartilage. Other joints can also be treated this way. This has been well studied with some clinical research having documented patient outcomes for over 15 years.
In short, the goal of regenerative stem cell-based biologics is to assist the local spinal or joint tissues to reduce the aging effects of chronic degenerating inflammation that leads to “osteoarthritis” which can lead people to what is sometimes referred to as “bone on bone” joint status. At the same time, stem cell and local bone and cartilage cells can then focus on producing healing proteins and related activities, like DNA repair, anti-oxidant production, and manufacturing of healthy, new cartilage.
It is exciting that our own bodies can heal and regenerate joint cartilage (and by extrapolation, disc cartilage) through regenerative medicine, with injection of the local bone being the most long-lasting and effective method. Benefits include reduced pain, improved movement, and avoidance of pills, cortisone shots, or surgery.
BiohackingCongress Team is very grateful to Jeffrey D. Gross, M.D., Stem Cell Whisperer at ReCELLebrate for joining the BiohackingCongress and giving a life-changing lecture.
Watch Jeffrey D. Gross’s 40-minute lecture and 100+ lectures, panel discussions, and performances from renowned biohackers on biohacking your body with a BiohackingCongress year-long subscription. Get your access to a healthy future now!
Subscribe to watch more Videos with Top Biohackers. Stay tuned into the latest biohacking products for biohacking your health and biohacking for longevity.
Based on the lecture by Dr. Jeffrey D. Gross
Special Access to
Exclusive TopBiohacks
and more


