The Gut Brain Axis: Exploring and Restoring with Microbiome Labs
“Your nervous system is in direct contact with your brain communicating via the vagus nerve helping your brain understand what's passing through, the lumen, food and water. Different levels of information are being communicated from the gut to the brain continuously. There are immunological responses between the gut and the brain, there's lots of communication going back and forth and so there are actually more neurons in the gut than there are in the entire spinal cord.
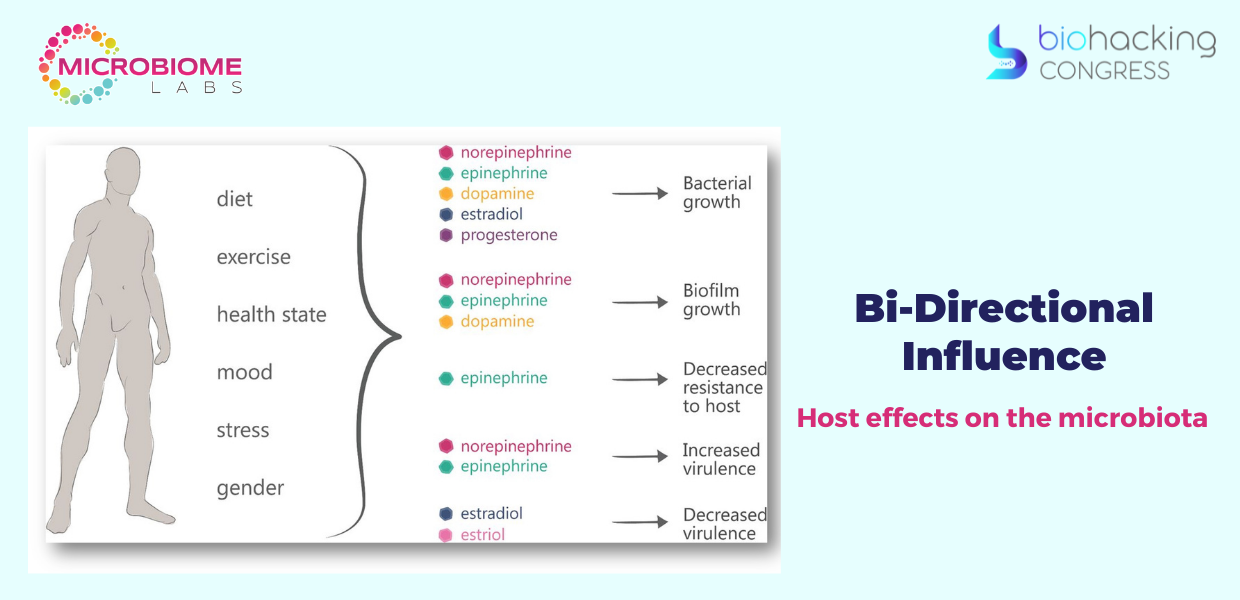
The microbiome itself has a bidirectional influence on our bodies and particularly hormones and neurotransmitters so what we have is we know that diet, exercise, healthy state, mood, stress, and gender can have influences on these neurotransmitters and hormones. Those balances within those neurotransmitters and hormones give us particular benefits to the microbiome also though what we have is that the healthy microbiome can influence all of these things. We've got this symphony of neurochemicals and hormones that are moving back and forth throughout the body and helping the cells of your body understand what's happening and what the master plan is from the brain and this is how the communication between the gut and the brain is what's critically important to get these neurotransmitters and these hormones imbalance.
Host effects on the microbiota. A variety of host factors (such as diet, exercise, mood, general health state, stress and gender) lead to alterations in hormonal levels, which in turn lead to a variety of effects on the microbiota (including growth, virulence and resistance).
“Lipopolysaccharide is a normal occurring molecule in the membrane of gram-negative bacteria. Your digestive tract is full of gram-negative bacteria when they die, they lice, and when they lyse they release these LPS into the lumen of the intestines now normally it would go out in the stool and there would be no problem but when this lps spills into the circulation of your blood that's when you get a reaction.”
Healthy Gut Characteristics:
- High diversity and protective strains
- High production of SCFA
- Well formed tight-junctions

“The happy microbiome is going to start getting out of balance. There are going to be some pathogens that are going to show up and they're going to start penetrating the mucin layer. At this point, you've got bacteria laying on the epithelial surfaces one cell layer deep. Your body doesn't have the ability to see good bacteria versus bad bacteria. It just sees bacteria so now there's inflammation, now they start to see gaps in the tight junctions and we see the LPS building into the bloodstream along with other bacteria and bacterial byproducts. Your body thinks you're in a state of septicemia, a bacterial infection in your blood. The LPS makes its way to the vagus nerve, travels up to the brain and then deposits itself in the brain.
I'm going to present you the research that proves that cool little schematic that I just did - that's true.
- “Effects of gut-derived endotoxin on anxiety-like and repetitive behaviors in male and female mice” Christopher T. Fields, Benoit Chassaing, Alexandra Castillo-Ruiz., Remus Osan, Andrew T. Gewirtz & Geert de Vies: “In spite of the ubiquitous nature of LPS in the gut lumen, this is the first study to demonstrate that intestinally derived LPS can initiate behavioral aspects of the sickness response. While an increased enteric load of LPS increases anxiety-like behavior in both sexes, it likely does so via sex-specific mechanisms.”
- “Basal and LPS-stimulated inflammatory markers and the course of individual symptoms of depression” - Wessel A. van Eeden , Albert M. van Hemert, Ingrid V. E. Carlier, Brenda W. 1. H. Penninx, Femke Lamers, Eiko 1. Fried, Robert Schoevers & Erik J. Giltay: “We hypothesized that inflammation is predictive of the severity and the course of a subset of MDD symptoms, especially symptoms that overlap with sickness behavior, such as anhedonia, anorexia, low concentration, low energy, loss of libido, psychomotor slowness, irritability, and malaise.”
- “Cytokine production capacity in depression and anxiety” N Vogelzangs , P de Jonge, J H Smit, S Bahn & B W Penninx: “Results show that LPS-stimulated inflammation was associated with increased odds of current depressive/anxiety disorders (odds ratio (OR)=1.28, P=0.009), as was the case for basal inflammation (OR=1.28, P=0.001). “LPS-stimulated inflammation was associated with more severe depressive (β=0.129, P<0.001) and anxiety (β=0.165, P<0.001) symptoms, as was basal inflammation. Unlike basal inflammation, LPS-stimulated inflammation was still associated with (anxiety) symptom severity after adjustment for lifestyle and health (IDS: interleukin (IL)-8, MCP-1, MMP2; BAI: LPS index, IL-6, IL-8, IL-10, IL-18, MCP-1, MMP2, TNF-β).”
- “Altered Gut Microbiome and Intestinal Pathology in Parkinson's Disease” Han-Lin Chiang, Chin-Hsien Lin: “According to this conceptualization, the inflammatory response increases gut permeability and exposure to endotoxins or other bacterial products and induces α-synuclein aggregations, which in turn propagate to the CNS via the vagus nerve.”
How do you support a healthy gut barrier?
“We had healthy students at the university of North Texas and we fed them a high high caloric meal, and what we witnessed over over a number of hours at the five-hour mark after they ate, we saw a five to six x spike in LPS and now we have a system: we feed this person this high fat high calorie meal five hours afterwards we see a five to six x spike in LPS, we also know that that LPS that's now in their blood had to go from their gut to their blood. It had to go through that membrane into the bloodstream. We have our system to test, we have a human model for the leaky gut so we sent him home, no change in diet, no change in lifestyle, just 30 day supply of the probiotic and then come back, do the test meal again and let's test so check out what happened.
The effect of 30-days of probiotic supplementation on post-prandial responses to a high-fat meal. Principal Investigator: Brian K. McFarlin, PhD, FACSM, FTOS University of North Texas
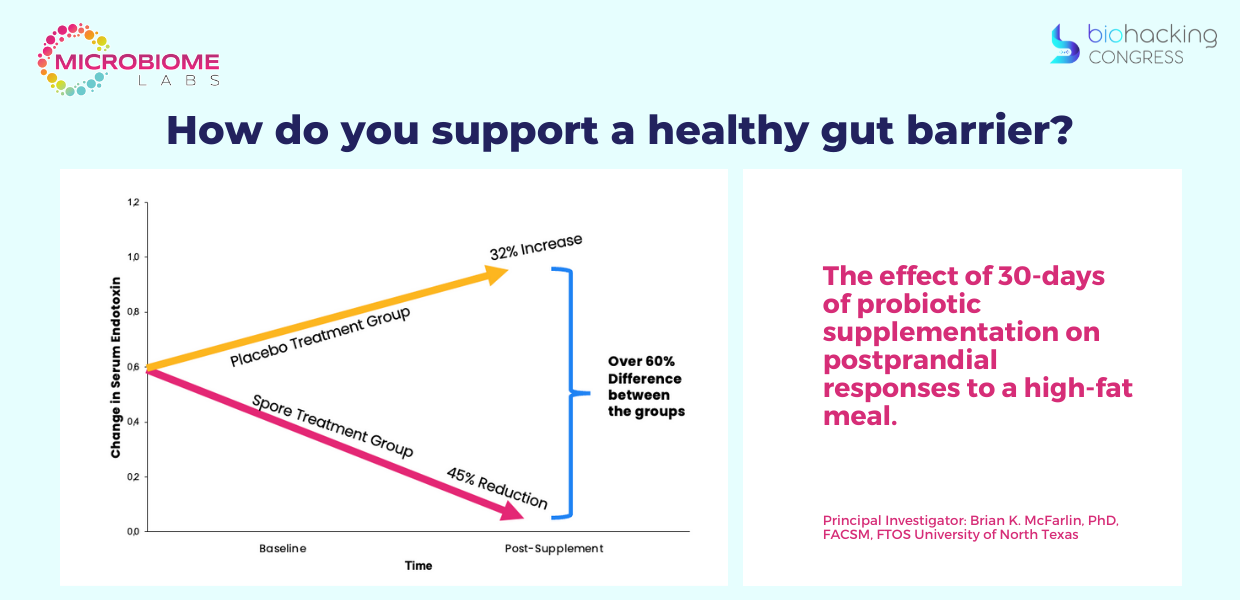
This is the first study that showed in fact we have a system where we can evaluate that the person has a leaky gut and we have a tool that can fix it.
MegaSporeBiotic is a probiotic blend of 5 Bacillus spores that have been shown to maintain a healthy gut barrier and immune function. The bi-phasic life cycle of the Bacillus spores allows them to remain dormant in harsh environments until they reach more favorable environments like the human gastrointestinal tract. Once inside the large intestine, these dormant spores can change into their active, vegetative forms and begin colonizing in the gut. This unique probiotic blend aims to RECONDITION the gut instead of reseeding with probiotic strains that cannot survive digestion or colonize the gut. MegaSporeBiotic has quickly become a household favorite among health practitioners and consumers alike.
Stress Induced HPA Activation
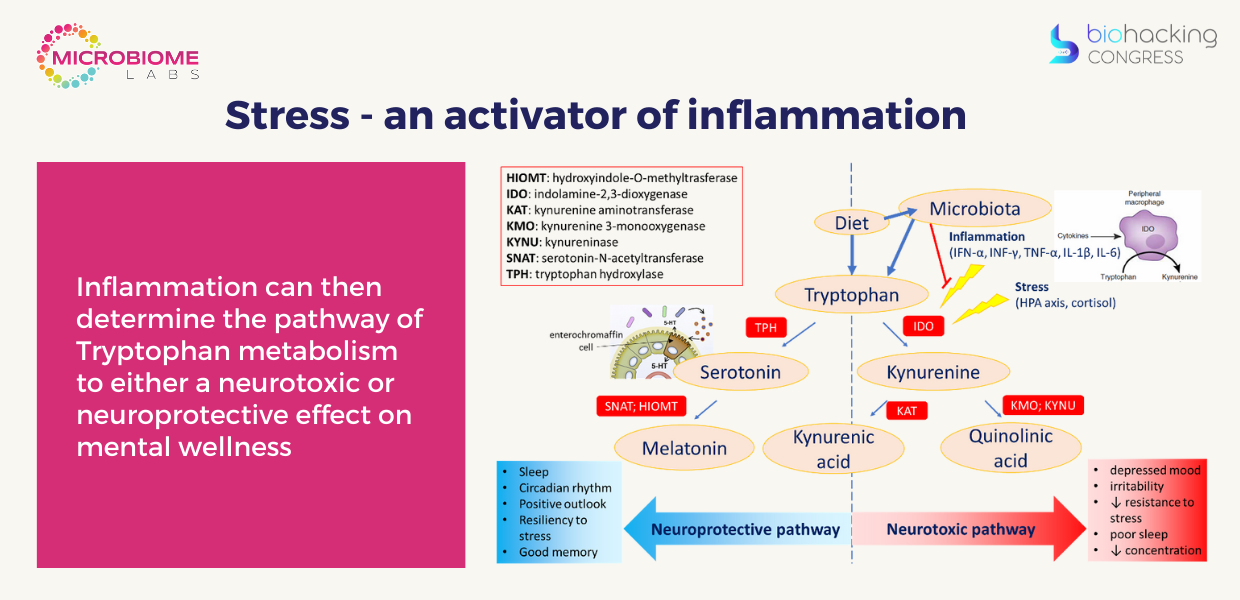
Stress - an activator of inflammation. Psychosocial stressors activate central nervous system stress circuitry, including CRH (Corticotropin-releasing hormone) and ultimately sympathetic nervous system outflow pathways
Acting through alpha and beta adrenergic receptors, catecholamines released from sympathetic nerve endings can increase NF-kB DNA binding in relevant immune cell types, including macrophages, resulting in the release of inflammatory mediators that promote inflammation.
- With increased levels of cortisol, there is an increase in the permeability of the gut wall (leaky gut), which then facilitates a systemic inflammatory response.
- A leaky gut drives a proinflammatory state as evidenced by increased levels of circulating TNF-α, interferon-γ, and IL-6.
- IL-6 is known to activate the HPA axis and over time it also down-regulates glucocorticoid receptors. These receptors are a feedback mechanism that suppresses the HPA axis, however, their downregulation results in a hyperactive and overly sensitive HPA axis.
- Evidence also suggests that these changes cause a reduction in hippocampal serotonin as well as a reduction in BDNF expression, all of which increase the susceptibility to depression. [Liang et al 2015] - Liang S, Wang T, Hu X, Luo J, Li W, Wu X, Duan Y, Jin F. Administration of Lactobacillus helveticus NS8 improves behavioral, cognitive, and biochemical aberrations caused by chronic restraint stress. Neuroscience.
- Inflammation can then determine the pathway of Tryptophan metabolism to either a neurotoxic or neuroprotective effect on mental wellness
How do you address stress induced HPA activation and inflammation?
Peptidoglycans - potential key regulators of gut microbiome-brain interactions with a role in neurodevelopment and behavior.
Pre-Clinical Conclusions on Inflammation. In 4 different animal studies:
- 1714® induces IL-10 cytokines (anti-inflammatory) in the spleen
- 1714® reduces the pro-inflammatory transcription factor NFκB in mice injected with LPS in a mouse endotoxemia model
- 1714® reduces the pro-inflammatory cytokines (IL-1β, IL-12p70, TNF-α) in serum or spleens in mice injected with LPS in a mouse endotoxemia model
- 1714® reduces the pro-inflammatory cytokines (IL-1β, IL-12p70, TNF-α) in mouse spleens in a diet induced obesity model.
1714 is an anti-inflammatory strain with potential to help with inflammation mediated stress
Human Clinical Trial Conclusion. Stress response:
1714® reduced perceived stress and cortisol output in healthy male volunteer and this was associated with a reduction in the proinflammatory tone of these subjects demonstrated through a decrease in pro-inflammatory cytokines (IL-1β, IL-6, TNF-α) in TLR stimulated whole blood from these subjects.
Covid Long Haulers: “Of particular interest was the dysregulated metabolism of tryptophan, characterized by a decrease in serotonin production coupled with accumulation of quinolinate in [long covid] patients. Quinolinate is an excitotoxin that hinders neuronal function through multiple mechanisms including acting as an NMDA receptor agonist, and it indirectly drives accumulation of glutamate. Of particular interest was the dysregulated metabolism of tryptophan, characterized by a decrease in serotonin production coupled with accumulation of quinolinate in [long covid] patients. Quinolinate is an excitotoxin that hinders neuronal function through multiple mechanisms including acting as an NMDA receptor agonist, and it indirectly drives accumulation of glutamate. Early preliminary & confidential data shows that 1714 could direct tryptophan metabolism away from the neurotoxic pathway (quinolinic acid) & towards the neuroprotective pathway (melatonin) through its anti-inflammatory action. We are scoping whether a reasonable next step from this research would be to conduct a 1714 interventional clinical trial in these long-covid patients.
The brain is profoundly affected by inflammation, which is likely the primary driver of cognitive dysfunction and the major cause of inflammation is a dysbiotic gut microbiome.
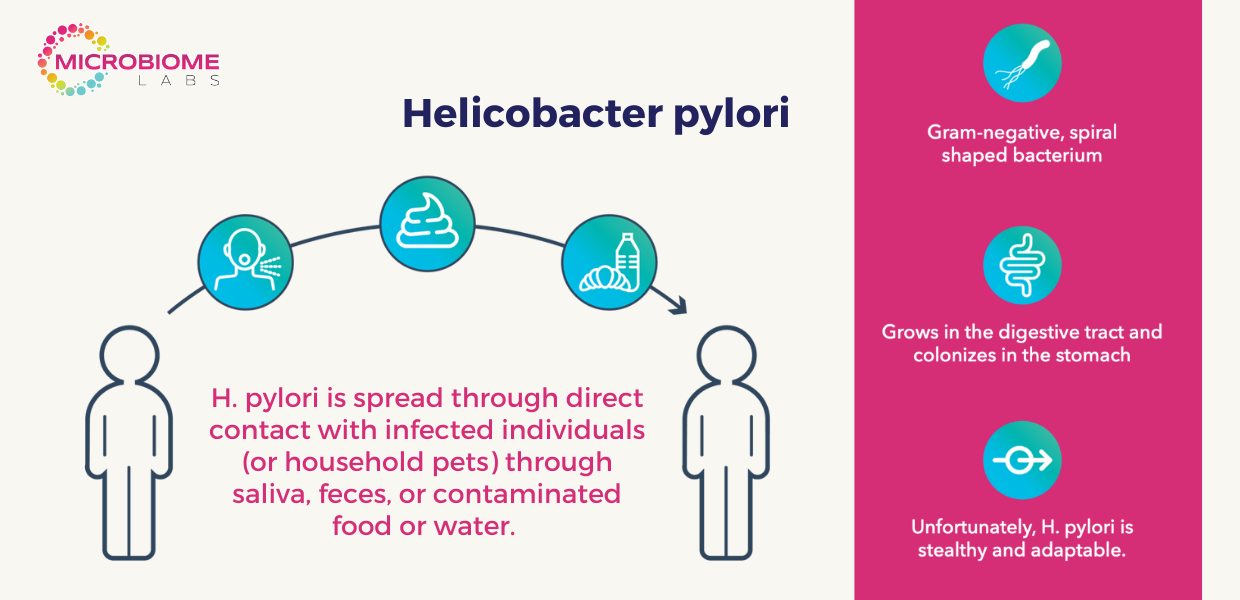
Helicobacter pylori
Helicobacter pylori (H. pylori) infection occurs when H. pylori bacteria infect your stomach. This usually happens during childhood. A common cause of stomach ulcers (peptic ulcers), H. pylori infection may be present in more than half the people in the world. Most people don't realize they have H. pylori infection because they never get sick from it.
H. pylori Alters Stomach Acidity:
- In the gastric mucosa, H. pylori can colonize and multiply.
- It works against the body’s defense mechanisms by secreting the enzyme urease, that converts urea to ammonia.
- H. pylori utilizes urea to produce ammonia and bicarbonate to raise the pH of the stomach.
- Thus, providing an optimal environment for H. pylori to reside and continue eroding stomach tissue.
The Problem and Common Symptomatology
An imbalance or overabundance with this bacterium can lead to detrimental pathologies such as chronic gastritis, peptic ulcer disease, gastric lymphoma, and gastric cancers.

Current Testing for H.pylori:
- Urea breath test (UBT) is often considered as the gold standard test in the diagnosis of H. pylori infection
- Stool testing
- Blood test
- Endoscopy
Current Treatment for H. pylori infection:
Most common approach: Triple therapy - It includes the use of stomach acid suppression with proton pump inhibitors (PPIs) and a course of two broad-spectrum antibiotics
Antibiotics
- Often cause unpleasant side effects like diarrhea
- Compliance to treatment can be low due to side effects
- Antibiotic resistance is an increasing problem
Proton Pump Inhibitors
- Individuals can become dependent on PPIs
- Omeprazole (a PPI) is among the top 10 most prescribed medications in the United States.
The use of PPIs have been shown to disrupt both the gastric and gut microbiomes. PPIs therapy profoundly inhibits gastric acid production leading to the proliferation of C Diff from its dormant state to its active, vegetative state.
Triple Therapy Microbial Effects
Triple treatment (TT) group: abundance and diversity of both intestinal bacteria and fungi decreased after 2 weeks of PCA (PPI, clarithromycin and amoxicillin) treatment, compared with those before treatment. TT plus probiotic treatment group received PCA followed by 6 weeks of the probiotics Bacillus Subtilis. No obvious changes were observed in abundance and diversity. Changes in the intestinal microbiota were more moderate after combined therapy with probiotics additives: Intestinal bacterial diversity was not substantially different from that of healthy persons at the tenth week, while intestinal fungal diversity was always similar to that of the HC group.
Benefits of PyloGuard™ by Microbiom Labs:
- Supports bacteria levels in the stomach
- Supports the microbiome
- Removes unwanted components from stomach
- Supports elimination of unwanted components in the gut
- Maintains H pylori levels already within the normal range
- Promotes the body’s process of elimination
BiohackingCongress Team is very grateful to Dr. Tom Bayne, President of Microbiome Labs for joining the BiohackingCongress and giving a life-changing lecture.
Watch Dr. Tom Bayne’s 40-minute lecture and 100+ lectures, panel discussions, and performances from renowned biohackers on biohacking your body with a BiohackingCongress year-long subscription. Get your access to a healthy future now!
Subscribe to watch more Videos with Top Biohackers. Stay tuned into the latest biohacking products for biohacking your health and biohacking for longevity.
Based on the lecture by Dr. Tom Bayne
Special Access to
Exclusive TopBiohacks
and more



